
A Guide to GLP-1-Based Medicines for Diabetes and Weight Management in Singapore
Obesity is a chronic, treatable neurometabolic disease that is projected to affect nearly a quarter of the world’s population by 2035. Until recently, advances in the development of pharmacotherapy for obesity were modest.
With the advent of GLP-1-based weight loss medications like Semaglutide and Tirzepatide, the treatment of obesity has been transformed. These medications are becoming more popular in Singapore as doctor-prescribed options for managing obesity and related health issues. They target hormonal pathways influencing appetite and metabolism, offering medical support where lifestyle changes alone may not be enough.
This guide outlines the different GLP-1-based medications available, how they work, the various benefits, and what to expect, helping you make informed decisions with guidance from a qualified doctor.
What Are GLP-1-Based Medications?
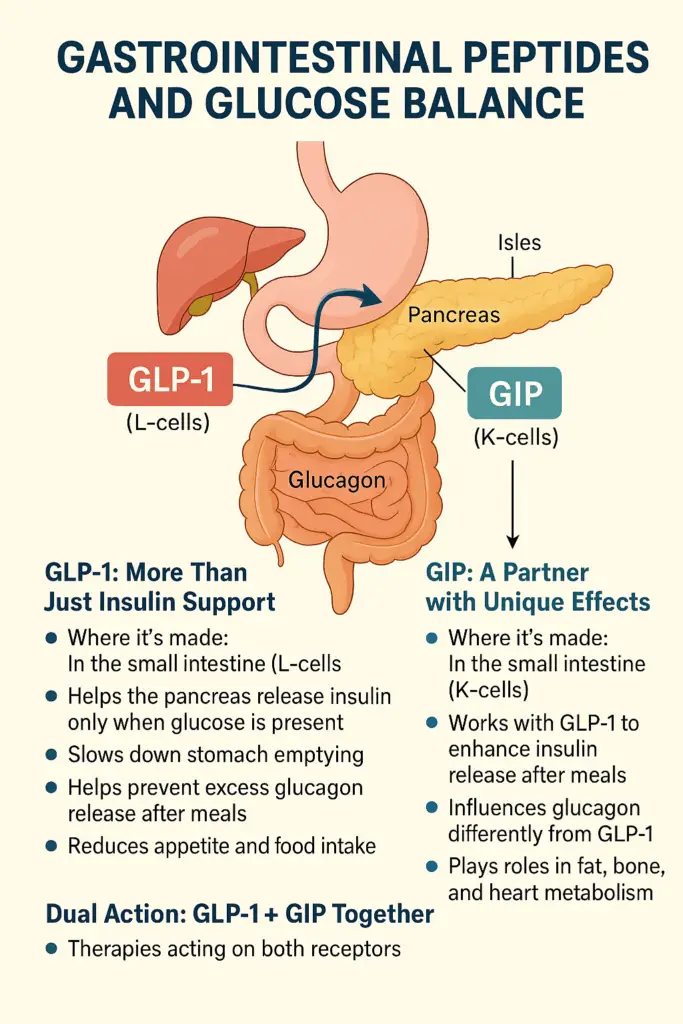
Alongside insulin and glucagon, special messengers from the gut called gastrointestinal peptides play a powerful role. Two of the most important ones are GLP-1 (Glucagon-Like-Peptide-1) and GIP (Glucose-dependent Insulinotropic Polypeptide). These are known as incretin hormones because they connect food intake with insulin release.
When you eat, GLP-1 and GIP are released from the small intestine in response to glucose, protein and fat. This is one of the body’s natural ways of linking meals to hormone signals that help control blood sugar and appetite.
Because natural GLP-1 breaks down quickly in the body, researchers developed GLP-1-based medications, otherwise known as GLP-1 receptor agonists (GLP1-RAs), that last longer and can be given once daily or once weekly. These medicines mimic the natural hormone but remain active for longer periods, helping with blood sugar management in type 2 diabetes1.
In clinical use, GLP-1-based medications have been prescribed for:
- Type 2 diabetes: To improve blood glucose control when used alongside diet, lifestyle measures and other forms of anti diabetic medications
- Weight management: In certain suitable individuals, as part of a structured plan under medical supervision
What Are the Different Types of GLP-1-Based Medications in Singapore?
GLP1-RA medications that are available in Singapore are semaglutide, liraglutide and dulaglutide. In addition, there are dual GLP-1/GIP receptor agonists such as tirzepatide. These dual GLP-1/GIP receptor agonists act on two hormone pathways for potentially greater weight loss and improvements in related conditions.
Semaglutide
Semaglutide is a GLP-1RA medication that is available in oral and injectable forms. It is used with diet and lifestyle changes for diabetes and weight management.
Tirzepatide
Tirzepatide is a dual GIP/GLP-1 receptor agonist. It activates two hormone receptors, glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide 1 (GLP-1), to regulate blood sugar, reduce appetite and induce weight loss. It is available as a weekly injection and is prescribed for individuals to assist with the management of their diabetes and weight management.
Liraglutide
Liraglutide is a once-daily injectable medication used for the management of diabetes and weight loss in adults with obesity or overweight and weight-related health conditions. It is also approved for use in adolescents aged 12 to 17 years with obesity and a body weight over 60kg.
Dulaglutide
Dulaglutide is a once weekly injectable medication that is used for the management of diabetes in conjunction with diet and lifestyle management, as well as other anti diabetic medications.
Benefits of GLP-1-Based Medications

Type 2 Diabetes Management
GLP-1-based treatments such as semaglutide2 3 4, tirzepatide5, liraglutide6 and dulaglutide were originally developed to treat type 2 diabetes7. They improve blood sugar control by lowering HbA1c levels and increasing the likelihood of reaching healthy glucose targets. Depending on the different types of GLP-1-based medications, HbA1C reduction has been shown to range between -0.7 and -2.5%.
Such injections achieve this through regulating insulin and glucagon levels in the blood. Additionally, they may help slow the progression of cardiovascular complications and diabetic kidney disease in individuals with type 2 diabetes7.
Weight Management
GLP-1-based treatments are now the first-line medications for weight management. Studies have shown that in combination with regular doctor monitoring and diet and lifestyle interventions, significant weight loss* has been observed:
- Semaglutide: Up to 15.8% over 68 weeks8 9
- Tirzepatide: Up to 22.5% over 72 weeks10
- Liraglutide: Up to 6% over 56 weeks8
*Results may vary according to the individual. Please seek a healthcare professional’s advice to understand which treatments are suitable.
Protecting Cardiovascular Health
Clinical trials have shown that semaglutide2 3 4, tirzepatide11 and liraglutide12 can significantly reduce the risk of heart failure, major cardiovascular events such as heart attack, stroke, and death. This benefit is seen in individuals with and without diabetes, particularly those with a history of cardiovascular disease.
Heart Failure Symptom Relief
In people with obesity-related heart failure, semaglutide13 and tirzepatide11 have been associated with improvements in symptoms such as fatigue, breathlessness, and swelling. It may also enhance physical function and exercise tolerance.
Reducing Progression of Kidney Disease
Individuals with chronic kidney disease with or without type 2 diabetes have been shown to experience a reduction in albuminuria with the use of semaglutide14.
Treatment of Obstructive Sleep Apnea
Among individuals with moderate to severe obstructive sleep apnea, tirzepatide15 was found to reduce the severity of obstructive sleep apnea through lowering body weight and blood pressure. This improved sleep-related patient-reported outcomes.
Other Possible Benefits Being Studied
There is currently evidence of promising results on the use of tirzepatide16 on metabolic dysfunction-associated steatohepatitis with liver fibrosis (fatty liver with fibrosis).
Side Effects and Risks of GLP-1-Based Medications
GLP-1-based treatments are generally well-tolerated and offer multiple health benefits, but like all medications, they can cause side effects. Most are mild and improve as your body adjusts, but some may require medical attention. These can include:
- Nausea, vomiting, or bloating
- Constipation, diarrhoea, or stomach discomfort
- Indigestion or heartburn
- Loss of appetite
- Feeling tired or weak
- Headache
- Redness, swelling, itching, or pain at the injection site
- Rarely, lumps or scarring may occur if injections are not rotated
In rare cases, more serious risks can occur and may require immediate medical attention. These include:
- Pancreatitis: Sudden severe stomach pain, nausea, or vomiting
- Gallbladder problems: Pain in the upper abdomen, yellowing of skin or eyes
- Kidney issues: Decreased urination, swelling, or rapid weight gain
- Low blood sugar (when used with insulin or sulfonylureas): Dizziness, sweating, confusion, shakiness
- Allergic reactions: Rash, swelling of the face or throat, difficulty breathing
- Mood or mental health changes: Depression, irritability, or suicidal thoughts
- Rare eye complications: A very small increased risk of non-arteritic ischemic optic neuropathy (NAION) has been reported
- Thyroid cancer: Unusual lumps in the neck, hoarseness, or trouble swallowing
It’s best to speak to your doctor before starting GLP-1-based treatments to understand the potential side effects and risks, especially if you have existing health conditions. Always report any unusual symptoms, and do not stop or adjust your medication without medical advice.
What to Keep in Mind When Using GLP-1-Based Medications
- Effectiveness varies: Some therapies may support more weight loss than others, but results differ from person to person.
- Side effects are possible: The most common are gastrointestinal (nausea, vomiting, diarrhoea and constipation). These often improve with time.
- Commitment is important: Medications are part of a long-term plan that includes lifestyle support.
- Cost and access: Many of these medicines are not available in generic form and may not be covered by insurance.
How to Administer GLP-1-Based Weight Loss Injections

Injectable GLP-1-based treatments such as semaglutide, tirzepatide or dulaglutide should be injected on the same day each week, at any time of day, with or without food. If you are using liraglutide, daily morning injections are generally recommended. Here are the general steps to administer a GLP-1-based injection:
Step 1: Gather your supplies
Prepare your GLP-1-based medication pen, a new needle, alcohol swabs, and a sharps disposal container. Wash your hands thoroughly with soap and water. Some medications, like dulaglutide, come with an autoinjector.
Step 2: Check the medication
Inspect the solution in the pen. It should be clear and colourless. Do not use the pen if the liquid is cloudy, discoloured, or contains particles. Prime your pen as instructed by your healthcare professional.
Step 3: Choose your injection site
Choose one of the recommended subcutaneous injection sites: Stomach (at least 5cm or a 3-finger breadth away from your belly button), front of the thigh, or back of the upper arm. Rotate sites weekly/daily to avoid skin irritation.
Step 4: Clean the area
Use an alcohol swab to clean the chosen injection site. Allow the area to dry before injecting.
Step 5: Inject the medication
Attach a new needle to the pen. Hold the pen at a 90-degree angle to your skin. Insert the needle swiftly and steadily. Press and hold the injection button until the full dose is delivered. Keep the needle in place for a few seconds before removing it to ensure complete delivery.
Step 6: Dispose of supplies
Carefully remove the needle and place it in a puncture-resistant sharps container. Do not reuse needles. Store the sharps container safely, away from children and pets.
If you are new to using GLP-1-based treatments, speak with your doctor to learn the proper technique of administering the injection. They can walk you through the process and answer any questions about your medication.
FAQs About GLP-1-Based Medications
Am I suitable for GLP-1-based medications for weight loss?
GLP-1-based medications are prescribed for the management of type 2 diabetes and weight management. These are strictly prescription-based treatments, and you will need to consult a doctor before starting these treatments.
For weight management, you may be suitable for semaglutide, tirzepatide or other GLP-1-based treatment if you have a BMI of 30 kg/m² or higher, or a BMI of 27 kg/m² with a weight-related condition such as high blood pressure, high cholesterol, or type 2 diabetes.
However, it is widely recognised that the World Health Organisation (WHO) definition of overweight and obesity for individuals of Asian ethnicity starts at a lower BMI level of 23 kg/m2 and 25 kg/m2, respectively. It is important to work with your doctors to understand your specific health needs and find the most suitable treatment.
In general, these treatments are intended for individuals who are unable to achieve significant weight loss through lifestyle changes alone. However, they are not recommended for everyone. Individuals who are pregnant or breastfeeding, have a history of certain thyroid conditions or pancreatitis, are generally not suitable.
Your doctor will assess your medical history, current health, and treatment goals before prescribing these injections and will provide ongoing monitoring to ensure the treatment is safe and effective for you.
Where can I buy GLP-1-based medications in Singapore?
GLP-1-based medications are available in Singapore through specialist public or private medical clinics like LG Endocrinology. These medications are prescription-only and cannot be purchased over the counter. You must first consult a doctor who will assess your suitability based on your health profile and treatment goals. Do be careful about purchasing medications online and without a doctor’s prescription, as fraudulent medications have been reported.
What is the price of GLP-1-based medications in Singapore?
In Singapore, the cost of GLP-1-based medications may vary according to the type and dose. Additionally, prices may vary between private clinics and do not include consultation, investigations and follow-up fees. Your doctor will recommend the most appropriate option based on your health needs and treatment goals.
When should I see an endocrinologist?
You should consider seeing an endocrinologist if you are struggling with weight loss despite lifestyle changes, or if you suspect your weight issues may be linked to a hormonal imbalance. Obesity is not just a matter of diet, as it can be influenced by conditions such as hypothyroidism, polycystic ovary syndrome (PCOS), insulin resistance, or Cushing’s syndrome.
If you’re facing challenges with weight management or have been diagnosed with a related condition, book an appointment with Dr Linsey to get the medical insight and support you need for long-term health.
Disclaimer
This information is provided for general education. It does not replace personalised medical advice. Please consult your doctor for guidance on the medications that may be appropriate for you.
Written by Dr Linsey Gani

Dr Linsey Gani is an endocrinologist experienced in weight management and metabolic health. She completed her residency in Melbourne, Australia and is a fellow of the Royal Australian College of Physicians and the Academy of Medicine, Singapore.
1 Nauck MA, Quast DR, Wefers J, Pfeiffer AFH. The evolving story of incretins (GIP and GLP-1) in metabolic and cardiovascular disease: A pathophysiological update. Diabetes Obes Metab 2021;23 Suppl 3:5-29.
2 Lincoff AM, Brown-Frandsen K, Colhoun HM, et al. Semaglutide and Cardiovascular Outcomes in Obesity without Diabetes. New England Journal of Medicine 2023;389:2221-32.
3 Marso SP, Bain SC, Consoli A, et al. Semaglutide and Cardiovascular Outcomes in Patients with Type 2 Diabetes. New England Journal of Medicine 2016;375:1834-44.
4 McGuire DK, Marx N, Mulvagh SL, et al. Oral Semaglutide and Cardiovascular Outcomes in High-Risk Type 2 Diabetes. New England Journal of Medicine 2025;392:2001-12.
5 Jastreboff AM, Roux CWl, Stefanski A, et al. Tirzepatide for Obesity Treatment and Diabetes Prevention. New England Journal of Medicine 2025;392:958-71.
6 Marso SP, Daniels GH, Brown-Frandsen K, et al. Liraglutide and Cardiovascular Outcomes in Type 2 Diabetes. New England Journal of Medicine 2016;375:311-22.
7 Pharmacologic Approaches to Glycemic Treatment: Standards of Care in Diabetes-2025. Diabetes Care 2025;48:S181-s206.
8 Committee ADAPP. 8. Obesity and Weight Management for the Prevention and Treatment of Type 2 Diabetes: Standards of Care in Diabetes–2024. Diabetes Care 2023;47:S145-S57.
9 Rubino DM, Greenway FL, Khalid U, et al. Effect of Weekly Subcutaneous Semaglutide vs Daily Liraglutide on Body Weight in Adults With Overweight or Obesity Without Diabetes: The STEP 8 Randomized Clinical Trial. Jama 2022;327:138-50.
10 Jastreboff AM, Aronne LJ, Ahmad NN, et al. Tirzepatide Once Weekly for the Treatment of Obesity. New England Journal of Medicine 2022;387:205-16.
11 Packer M, Zile MR, Kramer CM, et al. Tirzepatide for Heart Failure with Preserved Ejection Fraction and Obesity. New England Journal of Medicine 2025;392:427-37.
12 Marso SP, Daniels GH, Brown-Frandsen K, et al. Liraglutide and Cardiovascular Outcomes in Type 2 Diabetes. New England Journal of Medicine 2016;375:311-22.
13 Kosiborod MN, Abildstrøm SZ, Borlaug BA, et al. Semaglutide in Patients with Heart Failure with Preserved Ejection Fraction and Obesity. New England Journal of Medicine 2023;389:1069-84.
14 Perkovic V, Tuttle KR, Rossing P, et al. Effects of Semaglutide on Chronic Kidney Disease in Patients with Type 2 Diabetes. New England Journal of Medicine 2024;391:109-21.
15 Malhotra A, Grunstein RR, Fietze I, et al. Tirzepatide for the Treatment of Obstructive Sleep Apnea and Obesity. New England Journal of Medicine 2024;391:1193-205.
16 Loomba R, Hartman ML, Lawitz EJ, et al. Tirzepatide for Metabolic Dysfunction–Associated Steatohepatitis with Liver Fibrosis. New England Journal of Medicine 2024;391:299-310.
Related Articles
Insulin Pump Singapore: How It Works, Who Should Use It, and Costs
Insulin Pump Singapore: How It Works, Who Should Use It, and Costs Diabetes is common in Singapore, with 9.1% of

What Is Hormonal Acne: Causes, Treatment Methods and Prevention Tips
What Is Hormonal Acne: Causes, Treatment Methods and Prevention Tips Acne is more than just a surface-level skin concern. It

Erectile Dysfunction
Erectile Dysfunction Erectile dysfunction (ED) is more common than many people realize and can significantly impact an individual’s overall health
