Insulin Pump Singapore: How It Works, Who Should Use It, and Costs
Diabetes is common in Singapore, with 9.1% of Singaporeans aged 18 to 74 years living with the condition1. For individuals who require insulin, insulin pumps offer an alternative to multiple daily injections by delivering insulin continuously and more conveniently throughout the day.
Read on to learn more about the types of insulin pumps available in Singapore, who can benefit from them, and their associated costs. Additionally, learn how to use these devices and get answers to some frequently asked questions below.
What is an Insulin Pump?
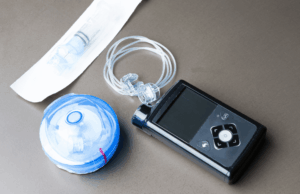
An insulin pump is a small, wearable device that delivers basal insulin continuously and bolus insulin at mealtimes through a thin tube known as a cannula. The cannula is inserted under the skin, usually in the abdomen.
Infusion sites are changed every 2 to 3 days. It is essential to rotate the insertion site regularly to prevent lipodystrophy, a condition characterised by the breakdown of fat tissue resulting from repeated insulin delivery in the same location.
What Are The Types of Insulin Pumps?
There are several types of insulin pumps available, each offering different features, levels of automation, and wearing styles. The main types are traditional tubed insulin pumps and patch (tubeless) pumps.
Traditional Tubed Insulin Pumps
Traditional insulin pumps consist of a small electronic device. Insulin flows from a reservoir through tubing to a small cannula placed under the skin. The pump itself is usually about the size of a small mobile phone and is worn on a belt, in a pocket, or attached to clothing.
These pumps require regular refilling using insulin cartridges and allow users to programme basal insulin delivery and administer bolus doses at mealtimes. While highly effective and customisable, they involve managing tubing and manual dose adjustments.
Insulin Patch Pumps
Insulin patch pumps are compact, wearable pods that deliver insulin directly under the skin. They are all-in-one, disposable devices that adhere directly to the skin, with no external tubing. They are smaller and lighter than traditional pumps, designed to be worn discreetly under clothing.
Patch pumps are controlled wirelessly using a handheld device or smartphone. Pods are also changed every 2 to 3 days.
Your healthcare team will help you choose a device based on your preferences, daily activities, and compatibility with glucose monitoring systems. There may be differences in the availability of traditional tubed insulin pumps and insulin patch pumps in different countries.
Automated Insulin Delivery (AID) and Hybrid Insulin Delivery Systems
Automated Insulin Delivery systems, also known as closed-loop or hybrid closed-loop systems, represent the most advanced form of insulin pump therapy. These systems combine three components: an insulin pump, a continuous glucose monitor (CGM), and a smart computer algorithm.
AID systems continuously monitor glucose levels and automatically adjust insulin delivery in response to rising or falling glucose trends. This helps reduce the risk of both hyperglycaemia and hypoglycaemia while improving overall glucose control.
By reducing the need for manual insulin calculations and frequent dose adjustments, AID systems significantly lower daily treatment burden. Hybrid closed-loop systems are now considered the standard of care for individuals with type 1 diabetes.
What Insulin Pumps Are Available in Singapore?
In Singapore, a range of traditional tubed insulin pumps is available to support individuals who require continuous insulin delivery. These pumps administer insulin through a tube and require users to programme basal rates and bolus doses based on meals and blood glucose readings.
Patch pumps, which are widely available internationally, provide a more discreet insulin delivery option. They are worn directly on the body and are typically controlled via a smartphone or a separate handheld device.
While traditional pumps and patch pumps differ in size, convenience, and method of use, both are designed to support effective insulin management. The most suitable option is typically determined through discussion with a doctor, taking into account medical needs, daily routines, and personal preferences.
Who Can Benefit from Insulin Pump Therapy?
Insulin pumps play an important role in diabetes management for those with type 1 diabetes who require regular insulin replacement. They may also benefit individuals with type 2 diabetes who need insulin to manage their blood sugar and prefer an alternative to multiple daily injections. Additionally, insulin pump therapy can be helpful for those who experience frequent hypoglycaemia, as it allows for more precise and flexible insulin dosing.
It is important to note that while insulin pump therapy can improve glucose management and reduce treatment burden, managing insulin levels is only one aspect of diabetes care. Combining insulin pump use with healthy habits and working closely with healthcare professionals to develop a comprehensive diabetes management plan can help maintain stable blood sugar levels and reduce the risk of long-term complications.
How Much Do Insulin Pumps Cost in Singapore?
Costs for traditional tubed insulin pumps vary depending on the brand and features such as hybrid closed-loop/CGM integration. There are also monthly consumable costs for tubed insulin pumps, although the base pumps can last from 4 to 7+ years.
Insulin patch pump costs are comparable to traditional tubed insulin pumps. Patch pumps are disposable and replaced every 2 to 3 days, so ongoing patch costs accumulate rapidly, similar to or possibly higher than traditional consumables over time (patch pricing varies by brand and supplier).
Subsidies and coverage may vary according to individual insurance policies and government subsidies. Training, ongoing follow-up, and support are essential for successful pump usage.
How to Use an Insulin Pump
Learning how to use your insulin pump effectively can help you manage diabetes more easily and safely on a day-to-day basis.
Getting Started
When you first start using an insulin pump, your doctor or endocrinologist will guide you on how to use it safely and effectively. They will set the initial pump settings and show you how to monitor your blood sugar and make adjustments when needed to maintain good glucose control.
Basal Insulin (Background Insulin)
Basal insulin is delivered continuously by the pump to manage blood sugar between meals. The delivery frequency can range from every 5 minutes to once an hour, depending on your pump and individual needs. Basal insulin may need to be adjusted during activities like exercise to reduce the risk of low blood sugar.
Bolus Insulin (Meal-time Insulin)
Bolus insulin is an extra dose given at mealtimes to manage carbohydrate intake. You calculate the carbs in your food and adjust your bolus dose accordingly. Pumps simplify bolus delivery, making it more accurate and convenient compared with manual injections.
Personalising Settings
Insulin pumps allow you to adjust key settings such as insulin sensitivity factor (ISF), duration of insulin action (DIA), and insulin-to-carbohydrate ratio (ICR). In addition, using a continuous glucose monitor (CGM) helps track glucose trends and support accurate dosing. If you’re physically active, insulin delivery can also be adjusted during exercise to prevent hypoglycemia.
FAQs About Insulin Pumps
How does a traditional insulin pump differ from a patch pump?
Traditional pumps use a separate device connected to a cannula under the skin. You will need to refill it and change the injection site every 2–3 days.
On the other hand, patch pumps are all-in-one devices that are stuck to the skin. They are disposable and need to be replaced every 1–3 days. These devices are smaller, lighter, and often easier to use, making them popular with many people with diabetes.
Do I need to check my blood glucose with an insulin pump?
Yes. Even when using a continuous glucose monitor (CGM), it is recommended to check your blood glucose level with a glucose meter before administering meal boluses or correction doses. Meter readings are important for safety and for adjusting CGM settings accurately.
Can I disconnect an insulin pump?
Yes, you can disconnect pumps with tubes for short periods, such as when showering, swimming, playing certain sports, or undergoing medical imaging (like X-rays).
However, the longer the pump is disconnected, the higher your blood glucose may rise. If disconnected for 2 hours or more, your risk of diabetic ketoacidosis (DKA)2 increases, which can be dangerous.
Can I shower with an insulin pump?
Some pumps with tubing are waterproof, but it’s best to check with the manufacturer. Many people find it easier to disconnect these pumps while showering and reconnect afterwards. For patch pumps, you can usually leave the device on while showering.
Disclaimer
This information is provided for general education. It does not replace personalised medical advice. Please consult your doctor for guidance on the medications that may be appropriate for you.
1Retrieved from Singapore Heart Foundation
2Diabetic ketoacidosis (DKA) is a serious complication that occurs when the body does not have enough insulin, causing blood glucose levels to rise and ketones to build up in the blood. This can lead to dehydration and electrolyte imbalance, and requires urgent medical treatment if not addressed promptly.

Dr Linsey Gani is an endocrinologist experienced in conditions related to hormonal imbalances, including those affecting fertility, menstrual health, and reproductive function. Dr Gani completed her residency in Melbourne, Australia. She is a fellow of the Royal Australian College of physician and the Academy of Medicine, Singapore.
Related Articles

What Is Hormonal Acne: Causes, Treatment Methods and Prevention Tips
What Is Hormonal Acne: Causes, Treatment Methods and Prevention Tips Acne is more than just a surface-level skin concern. It

A Guide to GLP-1-Based Medicines for Diabetes and Weight Management in Singapore
A Guide to GLP-1-Based Medicines for Diabetes and Weight Management in Singapore Obesity is a chronic, treatable neurometabolic disease that

Erectile Dysfunction
Erectile Dysfunction Erectile dysfunction (ED) is more common than many people realize and can significantly impact an individual’s overall health
