
What Is Hormonal Acne: Causes, Treatment Methods and Prevention Tips
Acne is more than just a surface-level skin concern. It reflects the complex interaction between hormones, skin glands, and inflammation. It develops when tiny hair follicles and sebaceous (oil) glands become overactive and inflamed.
Several key factors contribute to the formation of acne:
- Hormonal changes: Androgens stimulate the sebaceous glands to produce more oil, increasing the likelihood of blocked pores.
- Skin cell buildup: Dead skin cells accumulate and clog hair follicles, forming whiteheads and blackheads.
- Bacteria: Microorganisms like Cutibacterium acnes thrive in clogged pores and trigger inflammation.
- Genetic and lifestyle factors: Family history, diet, stress, and certain skincare habits can influence the severity and persistence of acne.
Dealing with persistent breakouts as an adult can be frustrating, especially when it feels like nothing you try makes a difference. Hormonal changes often play a role, making the skin unpredictable and difficult to manage. For many, these hormonal acne flare-ups are more than just a cosmetic concern. They can affect self-esteem and confidence, making everyday interactions and activities feel more stressful than they should.
The good news is that understanding the factors that trigger flare-ups and adopting the right approach can help reduce breakouts and restore control over your skin. In this article, we’ll be covering the key aspects of hormonal acne, including its causes, common symptoms, and prevention tips. We’ll also explore treatment options that can help reduce flare-ups and support healthier, clearer skin.
What Is Hormonal Acne?
Hormonal acne, also known as adult acne, commonly affects individuals between the ages of 20 and 50. It develops when fluctuations in hormone levels stimulate the oil glands to produce excess sebum. This overproduction clogs pores, which leads to breakouts.
While hormonal acne is more frequently seen in women, men can also experience it, particularly during puberty or if they have underlying hormonal disorders.
Hormonal acne may appear on the face, shoulders, chest, and back, and it often presents as:
- Pimples
- Blackheads
- Whiteheads
- Cysts
What Causes Hormonal Acne?
Hormonal acne is influenced by a combination of hormonal imbalances, lifestyle factors, and genetic predisposition.
Hormonal imbalances
Hormonal changes in the body are a major trigger for acne in both men and women.
- Menstruation, pregnancy, and menopause: Fluctuations in hormone levels during these periods can trigger hormonal acne.
- Discontinuation of birth control: Stopping hormonal contraceptives may cause changes in hormone levels, leading to breakouts.
- Testosterone treatment in men: Such treatments can increase oil production, potentially leading to acne.
- Polycystic ovary syndrome (PCOS) and other ovarian or metabolic disorders: These conditions can contribute to hormonal acne, often causing deeper, more painful lesions along the jawline and chin.
- Thyroid disorders: Hypothyroidism and hyperthyroidism may disrupt hormone balance, indirectly affecting androgens and worsening acne.
- Puberty and menstrual cycle: A surge in androgens during puberty increases oil production, while many women experience flare-ups just before their period due to cyclical hormonal changes.
Lifestyle factors
Daily habits and lifestyle choices can influence hormone levels and worsen acne.
- Stress: Stress raises cortisol levels, which stimulate sebum production and disrupt other hormones, worsening acne.
- Lack of sleep: Experiencing a lack of sleep disrupts hormone balance, increases inflammation, and may aggravate acne.
- Skincare and haircare products: Using products that are not oil-free, non-comedogenic, or non-acnegenic can clog pores and trigger breakouts.
- Diet: Refined sugars, processed foods, and high-glycaemic carbohydrates can raise insulin levels, stimulating androgen production and worsening acne.
Genetics and medications
Your genetics and certain medications can affect your risk of developing hormonal acne.
- Family history of acne: Genetic predisposition can affect how sebaceous glands respond to androgens and how the skin heals from acne, increasing the likelihood of hormonal acne.
- Certain medications: Steroids and other drugs that alter hormone levels may trigger acne.
How Is Hormonal Acne Diagnosed?
Diagnosing hormonal acne involves more than simply looking at breakouts on the skin. Doctors take a comprehensive approach to confirm whether hormones are the driving factor behind persistent or severe acne.
Clinical evaluation
Diagnosis usually begins with a physical examination. Your doctor will check for signs that point to hormonal acne, such as breakouts concentrated along the jawline, chin, and lower cheeks, or deep, painful cystic lesions.
A thorough review of your medical history is also important. This may include past skin conditions, hormonal disorders such as PCOS, family history of acne, current medications, and lifestyle factors like stress or sleep patterns.
Hormonal testing
If a hormonal imbalance is suspected, your doctor may recommend blood tests. These tests can measure androgen levels and help identify conditions such as PCOS or adrenal gland abnormalities. For example, PCOS can cause elevated androgens, irregular menstrual cycles, and insulin resistance, all of which can worsen acne.
Thyroid function tests may also be carried out, as thyroid disorders can disrupt hormone balance and contribute to acne flare-ups. If you suspect your acne may be hormone-related, consider booking a consultation with us to receive a tailored assessment and treatment plan.
What Are Some Treatment Methods for Hormonal Acne?
Managing hormonal acne often requires a tailored approach that addresses both the surface symptoms and the underlying hormonal imbalances. Treatment options range from topical creams to oral medications and professional in-clinic procedures, depending on the severity of the condition. The most suitable treatment will depend on your individual needs and will be recommended by your doctor.
Topical treatments
Topical medications may be recommended for mild to moderate acne. They work by unclogging pores, reducing bacteria, and controlling inflammation on the skin’s surface. Common options include:
- Retinoids (e.g. tretinoin): Retinoids promote skin cell turnover and prevent clogged pores.
- Benzoyl peroxide: Benzoyl peroxide kills acne-causing bacteria and reduces excess oil.
- Topical antibiotics (e.g. clindamycin, erythromycin): These medications are often used together with benzoyl peroxide to lower the risk of antibiotic resistance.
Oral medications
For moderate to severe or persistent hormonal acne, oral medications may be prescribed. These work internally to address hormonal imbalance, excess oil production, or bacterial overgrowth. Options may include:
- Oral contraceptives: Oral contraceptives are used to regulate hormones and reduce female adult acne.
- Anti-androgens (e.g. spironolactone, cyproterone acetate): These block androgen effects and lower sebum production.
- Oral antibiotics (e.g. doxycycline or minocycline): By reducing bacterial growth and inflammation, oral antibiotics help manage acne worsened by bacterial overgrowth.
Professional procedures
In some cases, dermatologists may recommend in-clinic treatments to better manage stubborn hormonal acne and enhance skin appearance. These procedures can reduce inflammation, kill acne-causing bacteria, and improve overall skin texture. Examples include:
- Laser therapy: Laser therapy is used in hormonal acne treatment to target bacteria, reduce inflammation, and improve acne scars.
- Chemical peels: These agents contain chemicals such as salicylic acid or glycolic acid to exfoliate skin and unclog pores.
- Light therapy: Using blue light and red light, light therapy kills bacteria, reduces inflammation and supports healing.
How to Prevent Hormonal Acne
While medical treatments are often necessary for managing hormonal acne, daily habits and preventive measures can also make a big difference. A consistent approach to skincare, diet management, and stress management helps reduce breakouts and maintain healthier skin over the long term.
Skincare
A consistent skincare routine is essential for keeping pores clear and reducing breakouts. Using the right products helps control oil, remove impurities, and protect the skin barrier. Key steps include:
- Using a mild, non-comedogenic cleanser with ingredients like salicylic acid
- Incorporating gentle exfoliation 2–3 times a week with AHAs or BHAs (chemical exfoliants that remove dead skin)
- Applying treatment products such as retinoids or benzoyl peroxide to regulate skin turnover and target bacteria
- Choosing a lightweight, oil-free moisturiser to maintain hydration
- Wearing daily sunscreen (SPF 30 or higher) to protect against damage and prevent post-acne marks
Diet
Dietary choices play a major role in hormonal balance and acne severity. Certain foods can trigger insulin spikes or inflammation, while others support more stable blood sugar levels and reduce flare-ups. Some dietary modifications that can help with achieving clearer skin are:
- Eating low glycaemic index foods such as whole grains, fruits, and legumes to prevent rapid blood sugar rises
- Including healthy fats rich in omega-3, such as fish, walnuts, and flaxseeds, which help reduce inflammation
- Avoiding or limiting dairy products, as they may worsen acne in some individuals
- Cutting back on sugary and processed foods that raise insulin and androgen levels, both of which can fuel acne
Stress management
Stress is a well-known trigger for hormonal acne, as it disrupts hormone balance and increases inflammation. Managing stress supports both hormonal stability and skin health. Helpful stress-relief strategies include:
- Practising mindfulness or meditation to calm the nervous system and lower stress levels
- Engaging in at least 150 minutes of moderate exercise weekly to regulate hormones and improve circulation
- Prioritising 7–9 hours of quality sleep each night to restore hormonal balance and reduce inflammation
FAQs About Hormonal Acne
What is the difference between regular acne and hormonal acne?
Acne is an inflammatory disorder of the pilosebaceous unit, which consists of the hair follicle and its associated sebaceous gland. Its pathogenesis is complex and involves multiple interacting factors, including androgen-mediated stimulation of the sebaceous glands, bacterial proliferation (Cutibacterium acnes), accumulation of dead skin cells, and various genetic and lifestyle influences.
On the other hand, hormonal acne is driven by fluctuations in hormone levels. It typically presents as deep, painful cysts or nodules along the jawline, chin, and lower face. It often flares up cyclically during menstruation, pregnancy, menopause, or in conditions such as PCOS, and is best managed with hormonal therapies, prescription medications, and lifestyle adjustments. Book an appointment with us today if you suspect you’re suffering from hormonal acne.
How long does hormonal acne last?
Hormonal acne can persist for several weeks to months, depending on the underlying hormonal fluctuations and individual factors. With an appropriate treatment plan, noticeable improvement is usually seen within 8 to 16 weeks.
Is hormonal acne a sign of menopause?
Yes, hormonal acne can be a sign of menopause. As women approach menopause, the body undergoes a gradual hormonal transition called perimenopause, during which estrogen levels decline more rapidly than testosterone. This relative excess of testosterone can increase sebum production, clog pores, and trigger acne.
While it can be frustrating, menopausal acne is common and manageable through a combination of lifestyle adjustments, skincare changes, and treatments such as topical or oral medications, and in some cases, menopausal hormone therapy to restore hormonal balance.
Can hormonal acne go away on its own?
Hormonal acne does not always go away on its own. While some people may notice improvements over time, this type of acne is often persistent and usually requires targeted treatments to manage effectively. Seeking treatment early is important to control breakouts and reduce the risk of acne scarring, which can be more difficult to treat later.
When should I see a doctor for hormonal acne?
You should consider seeing a doctor if your hormonal acne is persistent, worsening, or not responding to over-the-counter treatments. Professional help is also recommended for moderate to severe acne, such as deep cysts or inflamed lesions, which can lead to scarring if left untreated.
Additionally, you can consult a doctor if acne is affecting your self-esteem or causing pain. You can seek guidance on safe and effective treatment options, including prescription medications, hormonal therapy, or advanced procedures like laser or light therapy. If your acne isn’t improving, booking a consultation to seek advice early can help prevent long-term skin issues and achieve clearer, healthier skin.
Disclaimer
This information is provided for general education. It does not replace personalised medical advice. Please consult your doctor for guidance on the medications that may be appropriate for you.
Written by Dr Linsey Gani

Dr Linsey Gani is an endocrinologist experienced in conditions related to hormonal imbalances, including those affecting fertility, menstrual health, and reproductive function. Dr Gani completed her residency in Melbourne, Australia. She is a fellow of the Royal Australian College of physician and the Academy of Medicine, Singapore.
Related Articles
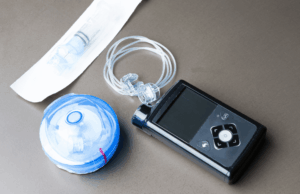
Insulin Pump Singapore: How It Works, Who Should Use It, and Costs
Insulin Pump Singapore: How It Works, Who Should Use It, and Costs Diabetes is common in Singapore, with 9.1% of

A Guide to GLP-1-Based Medicines for Diabetes and Weight Management in Singapore
A Guide to GLP-1-Based Medicines for Diabetes and Weight Management in Singapore Obesity is a chronic, treatable neurometabolic disease that

Erectile Dysfunction
Erectile Dysfunction Erectile dysfunction (ED) is more common than many people realize and can significantly impact an individual’s overall health
